During cold and flu season, excess mucus is a common, unpleasant symptom of illness, but the slippery substance is essential to human health. To better understand its many roles, researchers at the University of Utah’s John and Marcia Price College of Engineering synthesized the major component of mucus, the sugar-coated proteins called mucins, and discovered that changing the mucins of healthy cells to resemble those of cancer cells made healthy cells act more cancer-like.
Jessica Kramer, professor in the Department of Biomedical Engineering, presented the results of her group’s study at the spring meeting of the American Chemical Society (ACS).
“For hundreds of years, mucus was considered a waste material or just a simple barrier,” says Kramer. And indeed, it does serve as a barrier, regulating the transport of small molecules and particulates to underlying epithelial cells that line the respiratory and digestive tracts. But it also does much more. Studies show that mucus and mucins are biologically active, playing roles in immunity, cell behavior and defense against pathogens and cancer. Kramer’s team, for example, recently found that specific sugars attached to mucins inhibited coronavirus infection in cell culture.
“Part of the challenge of studying mucus and mucins in general is that they have quite a variety of protein structures,” Kramer explains. Although humans share more than 20 mucin genes, those genes are expressed differently in different tissues and are spliced to generate a range of proteins. In addition, cells modify those proteins in myriad ways with different sugars to meet the body’s needs.
Complicating the picture, genetic factors alone don’t determine mucin composition. Dietary and environmental factors can also influence which sugars become attached to these proteins. Thus, mucus composition can vary significantly from person to person, from day to day, and from tissue to tissue, all of which makes it difficult to identify the biological effects of any given mucin.
To study mucin properties, researchers can collect mucus from animals in slaughterhouses, Kramer says. “But ultimately, it’s quite labor intensive and difficult to purify. And in the process of doing the harvesting, usually the sticky, slimy properties are disrupted.”
As an alternative, mucins can be purchased off-the-shelf, Kramer explains. But because batch-to-batch variability can lead to problems with experimental reproducibility, methods are needed to reliably produce synthetic mucins at scale and at a reasonable price.
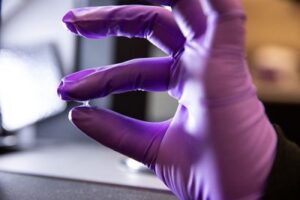
In the absence of a simple genetic method to produce individual mucins, Kramer’s lab combined synthetic chemistry and bacterial enzymes to generate the core polypeptides and then selectively add sugars to create unique synthetic mucins. This allows the researchers to test the physical, chemical and biological properties of individual types of mucin molecules and identify the impact of changing individual sugars or protein sequences.
Kramer, along with the lab of collaborator Jody Rosenblatt at King’s College London, is applying her team’s mucins to questions of cancer biology. In particular, the scientists are exploring the influence of mucins on the earliest stages of tumor formation. Previous studies in other labs have shown that mucins embedded in the surface of cancer cells promote metastasis, the spread of cancer to other tissues in the body. These mucins can also help the cancer cells evade immune system defenses by blocking immune cell activation.
“We are building synthetic mucins to understand how the chemical aspects of these proteins affect the behavior of cancer cells,” Kramer explains. “It hasn’t been possible to study these things before because we can’t control the molecular properties of mucins using traditional genetic and biochemical methods.”
Normally, as non-cancerous epithelial cells grow, they crowd together, with some getting eliminated from the epithelial layer to maintain a consistent and stable tissue structure. When Kramer’s team engineered the cells to have a bulky mucin-rich surface similar to that of cancer cells, the cells stopped extruding normally and piled up, forming what looked like the start of tumors.
Kramer is quick to note, however, that her team has not determined whether the genetics of the cells have changed, so they cannot yet state definitively whether the healthy cells were transformed into cancer cells. Those studies are ongoing.
The insights will be pivotal for the development of possible cancer treatments targeting mucins, as they will help highlight which parts of the mucin molecules are most important to tumor formation.
Scientists have been trying to make mucin-targeting therapeutics for decades, but that hasn’t worked well, in part because the sugar groups on the molecules weren’t fully taken into account, Kramer says. “For a vaccine, we can’t only consider the protein sequence because that’s not what the molecule looks like to the immune system. Instead, when an immune cell bumps into the surface of a cancer cell it’s going to see the sugars first, not the protein backbone.” So she believes an effective vaccine will need to target those mucin sugars.
Beyond cancer, the ability to reliably modify the protein sequence and sugars and produce scalable quantities of synthetic mucins offers opportunities to develop these molecules as anti-infectives, probiotics and therapies to support reproductive and women’s health, Kramer says.
The research was funded by the National Institute of General Medical Science, National Science Foundation and Marion Milligan Mason Fund.
Visit the ACS Spring 2024 program to learn more about this presentation, “Synthetic mucins: from new chemical routes to engineered cells,” and more scientific presentations. Read the original ACS press release here.